U.S. Health Insurance Claims Process (In-Network Services) ...U.S. Health Insurance Claims Process (In-Network Services) Flow Diagram
2025-03-07 18:37:01 218 2 Report 0
0
Login to view full content
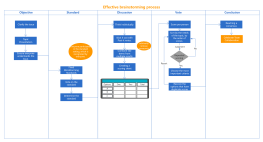
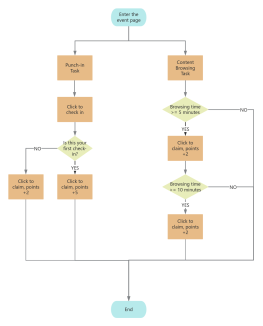
This flowchart illustrates the U.S. Health Insurance Claims Process for in-network services, detailing the interactions between key players such as healthcare providers, patients, and insurance providers. It begins with patient registration and insurance eligibility verification, progressing through medical coding, claims transmission, and adjudication. The flowchart highlights steps like receiving care, transcribing clinical notes into standardized codes, and reviewing claims. It also covers the issuance of explanations of benefits (EOBs) and remittance processing. This comprehensive guide serves as a valuable resource for understanding the intricate process of managing medical insurance claims within the U.S. healthcare system.
Other creations by the author
Outline/Content
NO
provide personal details and insurance information to Healthcare Provider
The claim is closed or ongoing (if further actions are needed).
healthcare provider sends a billto requesting payment
The key players and processes
transcribe notes and other clinical documentation into standardized medical codes.
Patient Medical Insurance Claim Process (In-Network Services)
EOB Issuance
confirm that the patient has adequate coverage for the care that they will receive
receive medical claims
send a payment to healthcare provider
If the patient owes?
Insurance eligibility verification
Payment and Notification Transmission
transmit medical claims
Private funding
resubmit the claim
insurance reviews the claim
Charge entry
Patient’s insurance provider(payor)
Healthcare providers
review and reformat medical claims
YES
Remittance Processing
Patient’s insurance provider
Claims transmission
A medical claims clearinghouse
send an explanation of benefits (EOB) to patient
healthcare providers makes notes in patient's medical record
providers or medical billing specialists list the charges that they expect to receive.
Patient pays a bill
Patient registration(check in)
send medical claims
Are the claimsaccepted?
Claims Appeals Management/Claims Denial Management
Receive care
Medical coding
Public funding(e.g. Medicare or Medicaid)
Patient statement
Claims Adjudication
Collect
Collect

Collect
0 Comments
Next page
Recommended for you
More